Discovery and Development: Spatial Omics
Harnessing spatial biology in drug discovery and development: navigating opportunities and challenges
How is current spatial biology being utilised in drug discovery and development for complex disease treatments, and how can it be improved?
Atanas Kamburov at Owkin
The pharmaceutical industry is under growing pressure to accelerate drug development timelines and improve patient outcomes, especially in complex diseases like cancer, autoimmune disorders and neurodegenerative diseases. Traditional methods of drug discovery have relied heavily on cell lines and other models. These have the advantage of being easy to interrogate, for example through genetic and chemical screening.
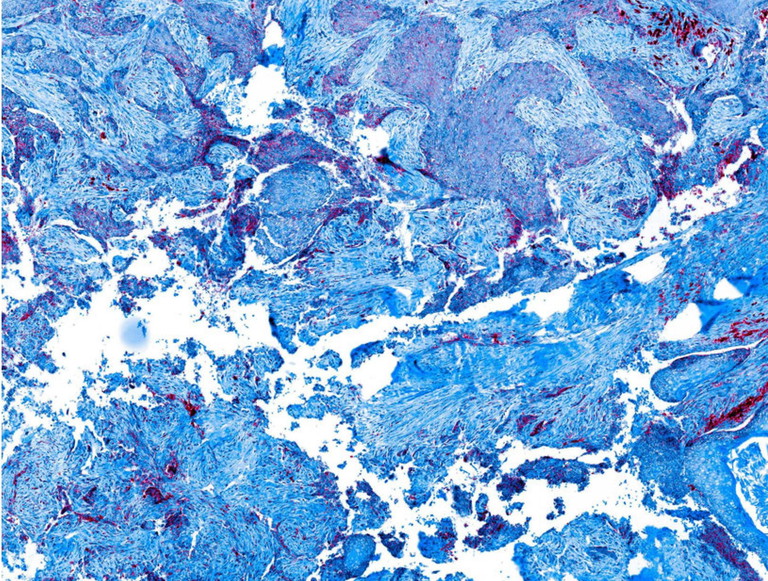
Model-based research has provided valuable insights and has led to the development of a number of novel drugs. However, many of the hypotheses it has generated did not translate to patients, mainly because models do not capture the complexity of diseases involving the immune system and generally the microenvironment of tumours. In addition, classical molecular biology approaches applied to human samples relied on genomics, transcriptomics and proteomics of the whole sample, falling short of delivering the level of detail needed to understand disease mechanisms at the cellular level. This limitation is especially evident in fields like immuno-oncology, where understanding the tumour microenvironment (TME) – how cancer cells interact with immune cells, stroma and blood vessels within tissues – is critical for developing new therapies.
Spatial biology, a rapidly emerging field that integrates molecular data with tissue architecture, offers the potential to transform drug discovery and development (DD&D) by providing unprecedented insights into how cells interact within tissues, and how some cells behave when they are spatially located close to other types of cells. Companies are now turning to spatial biology technologies to overcome some of the most pressing challenges in understanding disease progression, target validation and patient stratification.
Enabling the paradigm: spatial biology’s role in modern drug discovery
The advent of immuno-oncology has fundamentally changed how researchers approach cancer therapies. Instead of solely focusing on exploiting dependencies of tumour cells, scientists now aim to harness the body’s immune system to fight cancer. This shift requires a deeper understanding of the TME. Traditional techniques such as bulk RNA sequencing and single-cell RNA sequencing have provided valuable insights, but they lack the spatial context needed to truly understand these complex interactions. Spatial biology, on the other hand, allows researchers to visualise how cells behave in their native environments. For example, using spatial transcriptomics, researchers can map immune cell infiltration within a tumour and analyse how immune cells behave in close proximity to cancer cells and vice versa, how tumour cells infiltrated with immune cells are different from tumour cells in the same patient that aren’t infiltrated. This insight is critical for developing therapies that leverage the immune system to target tumours.
Another property inherent to cancers that is well captured through spatial biology approaches within their sampling range, but missed by traditional, bulk-based approaches, is intra-patient tumour heterogeneity. This heterogeneity can drive drug resistance, for example when one tumour clone responds to the drug but other resistant clones that survive under treatment with that drug exist alongside the sensitive one. Moreover, different, co-existing tumour clones can be infiltrated with different kinds of immune cells and to different degrees. Understanding of such heterogeneity, enabled by spatial transcriptomics, can guide the selection and positioning of combination treatments that aim to address all tumour clones and ecotypes/niches of a given patient at the same time. Organisations are increasingly exploring how spatial biology can enhance immuno-oncology research. By incorporating spatial data into their drug development pipelines, they aim to discover new biomarkers, identify drug targets and develop more personalised cancer treatments.
Expanding dimensionality: the next frontier in spatial biology
One of the most exciting advancements in spatial biology is the push to move beyond two-dimensional tissue sections, and study tissues in three dimensions. Current spatial transcriptomics technologies typically analyse thin tissue layers, which provide valuable but incomplete data on cellular behaviour. To gain a more comprehensive understanding of tissue architecture, researchers are now working to develop techniques that allow for the analysis of thicker tissue sections – up to 200 micrometres.
This three-dimensional analysis would enable researchers to study complex processes such as tumour metastasis, immune cell migration and tissue regeneration in greater detail. Additionally, adding a temporal dimension – observing how cells and tissues change over time – opens new possibilities for drug discovery. Imagine being able to track how tumour cells evolve and develop drug resistance in real time. Although this technology is still in its early stages, organisations are already exploring the development of ex vivo tissue models that simulate disease progression. These models could allow researchers to observe how cells respond to drugs over time, providing a more dynamic and comprehensive view of disease biology.
“By integrating spatial data into DD&D pipelines, companies can gain deeper insights into disease biology, improve the translatability of biological hypotheses into effective drugs in the clinic, and enhance patient stratification and the positioning of drugs and drug combinations in different patient populations”
Industry challenges: cost, complexity and standardisation
Despite its promise, spatial biology is not without challenges. The high cost and technical complexity of these technologies remain significant barriers to widespread adoption in both preclinical and clinical settings. For example, while spatial omics technologies provide rich data, they also generate vast amounts of complex information that require specialised analysis tools and expertise. This complexity can make it difficult for smaller companies or academic institutions to fully utilise these technologies.
Moreover, the sheer volume of data generated through spatial omics technologies can be overwhelming. With the improvement of these technologies, in terms of spatial resolution and number of features measured, or with the integration of spatial data with other types of data – such as single-cell transcriptomics or pathology imaging data – complexity is increased even more. To navigate this complexity, advanced analytics tools such as artificial intelligence are needed.
Standardisation is another pressing issue. As spatial biology technologies continue to evolve, there is a growing need for standardised analysis tools, file formats and data platforms. Currently, different technologies produce data in different formats, making it challenging to integrate findings across studies or across companies. The development of interoperable platforms that can harmonise spatial data will require collaborative efforts across the pharmaceutical, diagnostic and technology sectors.
Collaborative solutions: the path forward
To overcome these challenges, the industry must embrace collaboration. Consortia and partnerships between pharmaceutical companies, academic institutions and technology providers will be key to driving innovation. Efforts are also being made to reduce the cost and complexity of spatial biology platforms, making them more accessible for routine use. Automated spatial analysis systems, for instance, could allow clinicians to analyse patient samples more efficiently, enabling more precise diagnoses and treatment plans.
Conclusion: unlocking the full potential of spatial biology
Spatial biology represents a significant leap forward in our ability to understand complex disease mechanisms and develop more targeted, effective therapies. By integrating spatial data into DD&D pipelines, companies can gain deeper insights into disease biology, improve the translatability of biological hypotheses into effective drugs in the clinic, and enhance patient stratification and the positioning of drugs and drug combinations in different patient populations. However, realising the full potential of spatial biology will require overcoming significant challenges related to cost, complexity and standardisation.
The future of drug discovery is spatial, and organisations that can successfully harness this technology will be well-positioned to lead the next wave of innovation in healthcare. By fostering collaboration, investing in scalable solutions and working toward industrywide standardisation, the pharmaceutical industry can unlock the transformative power of spatial biology, ultimately improving patient outcomes and driving the future of precision medicine.

Atanas Kamburov is head of Pharma Solutions Data Science at Owkin. He has a PhD from the Free University of Berlin, Germany, where he focused on elucidating complex disease mechanisms through computational approaches. At Owkin, he has played a key role in initiatives like the MOSAIC project, which leverages spatial multi-omic technologies to create detailed cancer atlases, aiming to revolutionise our understanding of tumour microenvironments.